GW Physicians Talk About Advanced Care on the Front Lines
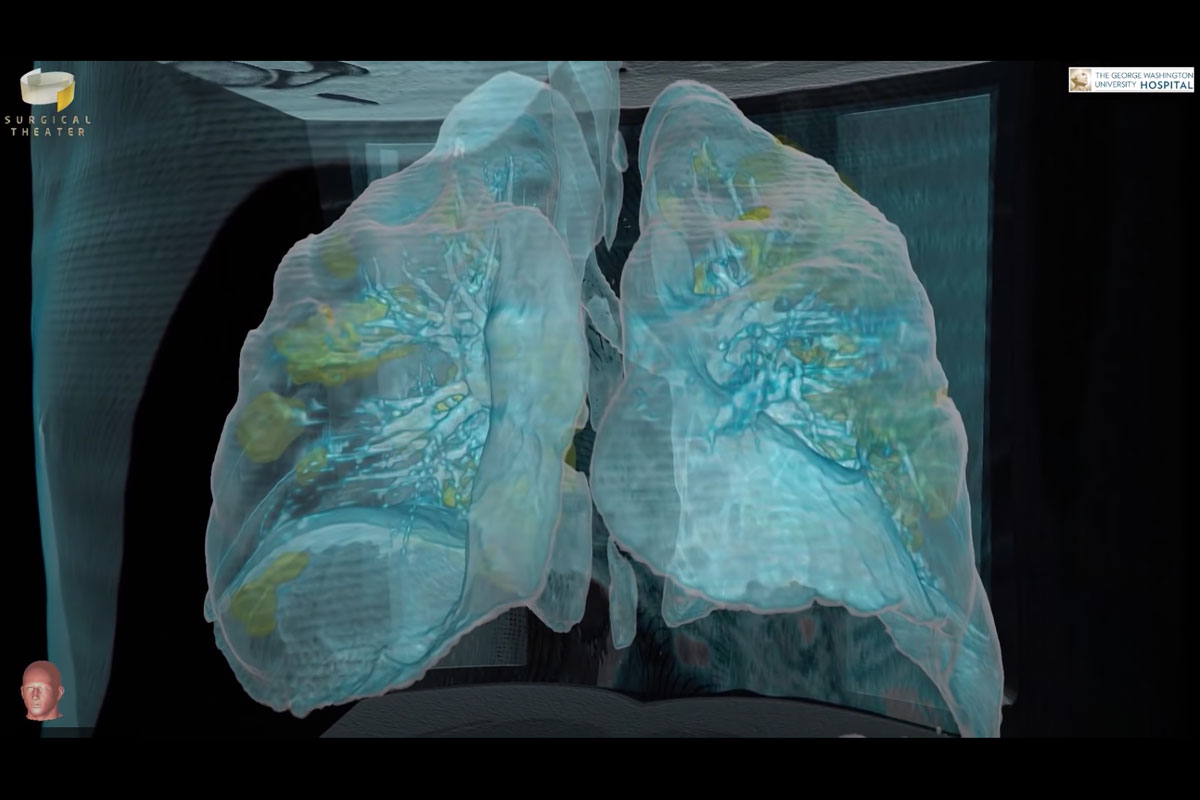
Virtual reality technology allows GW physicians to "see" and
assess the damage to the lungs of COVID-19 patients.
August 25, 2020
As the world unites in the battle against COVID-19, doctors at GW Hospital are using advanced technology and expertise to gain more insight into this novel virus, offering a vital chance at recovery for some of the most critically ill patients in the region.
Well before the first COVID-19-positive patient arrived at GW Hospital on March 18, the hospital was readying its teams and resources – including its Thoracic Surgery team, which would play a vital role in educating the nation and the world about the impact the virus has on the lungs. Cardiac surgeons, respiratory therapists and other specialists were also ramping up their capacity to provide advanced care for any patients with COVID-19 that may need it.
Specialty Care: Offering Vital Support With ECMO
The first COVID-19 patient at GW Hospital was a man in his late 50s whose only underlying medical condition was high blood pressure. He initially developed fever and cough, which progressed rapidly to severe shortness of breath. He was taken to a local hospital, where he was intubated and put on a mechanical ventilator. He needed higher and higher levels of support from that ventilator, and it got to the point where he was on maximal support but his condition continued to worsen. That was when the outside hospital reached out to the expert team at GW Hospital and arranged a transfer so the patient could receive an advanced heart-lung therapy called ECMO (extracorporeal membrane oxygenation).

ECMO is offered only at select facilities worldwide and provides a last treatment option when other treatments, including ventilators, are not helping the patient. Nothing about ECMO is simple. It requires a full operation with specially trained staff to place a patient on an ECMO machine and an entire team of specialists to take care of that patient. But it accomplishes something remarkable, taking blood out of the body, putting oxygen in, removing toxins (such as carbon dioxide) and returning the blood back to the body. While ECMO doesn’t treat the underlying issue, it temporarily does the work of the heart, lungs or both, providing critical time for healing, explains Cardiac Surgeon Elizabeth Pocock, MD.
ECMO is a potentially lifesaving technology for patients without other options and has proven successful in treating certain COVID-19 patients. However, despite the collaboration of the ECMO team and leveraging of all available resources, GW Hospital’s first COVID-19 patient lost his life to the virus.
"We've been doing ECMO for about 12 years, so we're used to taking care of critically ill patients," said Dr. Pocock. But COVID-19 has shown distinct challenges. "What I noticed specifically that is different about COVID patients is they come in and they have this catastrophic pneumonia for which we will place them on ECMO," she explained. "What we find is that the time they remain critically ill is really significant – not just days, but weeks. That is unusual."
 After a few weeks, some patients diagnosed with COVID-19 start having serious complications, including heart problems. "Some folks will start to develop changes of their heart, which is a sign that the virus is infiltrating the heart (also known as "myocarditis"). This is generally a very severe, high-mortality problem to have," Dr. Pocock said.
After a few weeks, some patients diagnosed with COVID-19 start having serious complications, including heart problems. "Some folks will start to develop changes of their heart, which is a sign that the virus is infiltrating the heart (also known as "myocarditis"). This is generally a very severe, high-mortality problem to have," Dr. Pocock said.
"In our experience, the surprise with COVID-19 patients on ECMO is how intense the inflammatory response is, how virulent, how fatal the infection can be," added Chief of Cardiac Surgery Farzad Najam, MD.
Discovery: Seeing Inside the Lungs With Virtual Reality Technology
 From the outset of the pandemic, it was clear that the lungs can be severely impacted by the virus. This was a key focus of the Thoracic Surgery team, led by Keith Mortman, MD, Chief of Thoracic Surgery, when the first COVID-19 patient arrived at GW Hospital for treatment. To better understand his condition and the disease progression while he was at the hospital, they used virtual reality (VR) technology to capture 360-degree images of his lungs. Doctors at GW Hospital have been using VR for nearly five years as a surgical planning and education tool for brain surgery and were the first in the nation to use VR for thoracic cases, including lung cancer care. Virtual reality uses images created from a CT scan to allow doctors to virtually step inside a patient for a detailed view. Aided by this technology, Dr. Mortman was deeply concerned by the extent of damaged lung tissue as a result of COVID-19.
From the outset of the pandemic, it was clear that the lungs can be severely impacted by the virus. This was a key focus of the Thoracic Surgery team, led by Keith Mortman, MD, Chief of Thoracic Surgery, when the first COVID-19 patient arrived at GW Hospital for treatment. To better understand his condition and the disease progression while he was at the hospital, they used virtual reality (VR) technology to capture 360-degree images of his lungs. Doctors at GW Hospital have been using VR for nearly five years as a surgical planning and education tool for brain surgery and were the first in the nation to use VR for thoracic cases, including lung cancer care. Virtual reality uses images created from a CT scan to allow doctors to virtually step inside a patient for a detailed view. Aided by this technology, Dr. Mortman was deeply concerned by the extent of damaged lung tissue as a result of COVID-19.
The images and a related podcast with Dr. Mortman's observations were quickly shared publicly to help educate people about the seriousness of COVID-19. An animation of the images – which shows lung tissue damaged by COVID-19 highlighted in yellow – illustrated the disease's terrible toll on the body. The VR images of COVID-damaged lungs were shared on local and national news media, including CNN and The New York Times, and circulated via media outlets throughout the world.
Collaboration: Teaming Up for Better Care
While the impact of COVID-19 has been felt worldwide, the doctors and staff at GW Hospital remain unwavering in their resolve to overcome this pandemic, and the collaboration among different specialties is inspiring. This includes discussions with Dr. Mortman and the Thoracic Surgery team about ways to harness VR technology to improve and advance patient care, said Dr. Pocock.
The highly contagious nature of the novel coronavirus can pose extra challenges and risks, but the providers at GW Hospital are prepared and rising to the challenge. "This is very much part of our job – a sacrifice we are absolutely willing to take," said Dr. Pocock. "This is why we chose to go into this field, for exactly this purpose, to try to save as many lives as we can."